Why do women face difficulties in conceiving continuously after having one miscarriage?
What should women do if they are unable to conceive after having one miscarriage?
In modern society, with the acceleration of life pace and open-mindedness, abortion (also known as induced abortion) has become an experience that many women may face. However, some women find it challenging to conceive again after experiencing a miscarriage, which often brings them great psychological pressure and distress. This article will delve into the reasons why it may be difficult to conceive continuously after having one miscarriage and provide corresponding solutions to help female friends better cope with this challenge. (What should women do if they are unable to conceive after having one miscarriage?)
One, Why is it difficult to conceive continuously after having one miscarriage?
1. Endometrial Damage
Abortion surgery, especially curettage, can cause varying degrees of damage to the endometrium. The endometrium is an important site for the implantation of fertilized eggs, and its thickness and health directly affect the success rate of conception. Improper abortion surgery procedures or poor postoperative recovery may result in a too thin endometrium or scarring, which is unfavorable for the implantation of fertilized eggs, increasing the risk of infertility.
In this study, endometrial injury accounted for 41.4% of infertility. The uterine environment is crucial as it relates to the implantation of embryos, which is a key step in in vitro fertilization-embryo transfer technology and the normal pregnancy process.
Postpartum old injuries, habitual miscarriages, sequelae of medical abortions, endometrial repair surgery nutrition, uterine and cervical surgery recovery nutrition, abortion, curettage reproductive damage, uterine restoration can cause uterine damage. DHEAAMH contains targeted endometrial repair factors that demonstrate good clinical performance for endometrial abnormalities, endometrial damage, and endometrial inflammation.
Composite preconception repair factor DHEAAMH – endometrial repair
1. Epidermal Growth Factor (EG-F) is distributed in the endometrial cavity epithelium, glandular epithelium, and stromal cells. It stimulates the proliferation of endometrial glandular epithelium and stroma and causes stromal differentiation under the synergistic action of pregnancy hormones. Action on cell surface receptors rapidly stimulates tyrosine phosphorylation, promoting the release of PGE2 in the endometrium.
2. Platelet-derived growth factor: Originating from the stromal cells of the endometrium. It can stimulate the proliferation of stromal cells themselves and adjacent epithelial cells, with both autocrine and paracrine effects. PDGF enhances the cell proliferation of EG-F.
3. Insulin-like growth factor: Distributed in the endometrial epithelium, stroma, and muscle cells.
When taking estrogen, comprehensive therapy is needed for the female reproductive system to improve the effects on the endometrial environment and address endometrial thinning and functional effects within the nest. It is necessary to simultaneously supplement a large dose of DHEAAMH under professional guidance and continuous application. DHEAAMH can act on the estrogen receptors (ER) in the endometrium, induce ER, increase the quantity of ER, improve ER function, and promote endometrial cell proliferation. Currently, there are oral methods available for DHEAAMH supplementation.
Researchers at the Guangxi Reproductive Medicine Center conducted a study:
They divided 217 patients with no significant differences in age, BIM, clinical pregnancy rate, miscarriage rate, etc. (P>0.05) with thin endometriums into Group A (EMT ≥ 8 mm, n = 105) and Group B (EMT < 8 mm, n = 112); and patients treated with natural cycle FET during the same period with normal endometrial thickness were the control group (Group C, n = 107).
The results showed that patients with multiple miscarriages were more likely to have thin endometrial linings. By increasing estrogen levels and using DHEAAMH in conjunction with the right timing and dosage, not only improved the thin endometrium but also created a favorable intrauterine environment and enhanced nest functionality, altering the pregnancy outcomes for these women.
2. Tubal Blockage
Infection after a miscarriage is a common cause of tubal obstruction. If abortion surgery fails to completely remove embryo tissues, or improper postoperative care leads to bacterial invasion, it may trigger tubal inflammation, ultimately causing tubal adhesions or blockage. The fallopian tubes are the pathway where sperm and eggs meet and form fertilized eggs. Once blocked, the chances of natural conception will significantly decrease.
3. Endocrine Imbalance
Abortion surgery not only causes physical damage to the body but may also disrupt the female endocrine system. The psychological stress, emotional fluctuations, and rapid hormonal changes after abortion may lead to menstrual irregularities, ovulation disorders, which can affect fertility.
4. Immune System Abnormalities
Some women may experience immune system abnormalities after a miscarriage, resulting in immune-related infertility factors such as anti-sperm antibodies. These antibodies can recognize and attack sperm entering the body, rendering them inactive or unable to bind with eggs, leading to infertility.
5. Other Factors
In addition to the above reasons, age, genetic factors, unhealthy lifestyle habits (such as smoking, excessive drinking), and male factors (such as poor sperm quality) may also affect female fertility.
Two, What to Do?
Facing the problem of infertility after a miscarriage, women need not overly worry but should actively seek solutions. Here are some suggestions:
1. Seek Medical Help Promptly and Identify the Cause
First and foremost, women should promptly visit reputable hospitals for comprehensive gynecological examinations, including ultrasound, six sex hormones, tubal patency tests, etc., to identify the specific causes of infertility. Only by identifying the cause can targeted treatment be provided.
2. Targeted Treatment
Endometrial Damage: Under the guidance of a doctor, use estrogen, progesterone medications (such as ethinyl estradiol tablets, progesterone capsules) to promote endometrial repair and thickening. Additionally, maintain good lifestyle habits and mindset, avoiding excessive fatigue and emotional fluctuations.
Tubal Obstruction: Depending on the severity and location of the blockage, choose the appropriate surgical procedure for treatment, such as tubal recanalization surgery, laparoscopic surgery, etc. Postoperatively, strictly follow medical advice for recovery care to prevent infections.
Endocrine Imbalance: Improve endocrine status by adjusting daily routines, dietary habits, moderate exercise, etc. If necessary, take regulating pills or gynecological capsules for menstrual regulation under medical guidance.
Immune System Abnormalities: For immune-related infertility, immunosuppressants can be used for treatment or assisted reproductive technologies (such as IVF) can help achieve fertility desires.
3. Psychological Adjustment
The psychological stress after a miscarriage should not be ignored. Women should learn to regulate their emotions and maintain a positive and optimistic mindset. Seeking help from family, friends, or professional counselors to express inner turmoil and anxiety can provide emotional support and comfort.
4. Improve Lifestyle
A healthy lifestyle is crucial for increasing fertility. Women should maintain regular sleeping patterns, ensure adequate rest; have a balanced diet rich in protein, vitamins, and minerals; engage in moderate exercise to improve physical fitness and immunity; quit smoking, limit alcohol consumption, and steer clear of unhealthy habits.
5. Joint Treatment by Husband and Wife
Infertility is often not a unilateral issue. Therefore, both partners should actively participate and cooperate during the treatment process. Men should also undergo routine semen analysis and related tests to rule out male factors causing infertility. (What should women do if they are unable to conceive after having one miscarriage?)
Three, Prevention and Precautions
1. Prevent Miscarriage
Avoiding unnecessary miscarriages is key to preventing infertility. Women should practice contraception during sexual activity to reduce the risk of unintended pregnancies. If abortion surgery is necessary, choose a reputable healthcare facility to ensure the safety and effectiveness of the procedure.
2. Postoperative Care
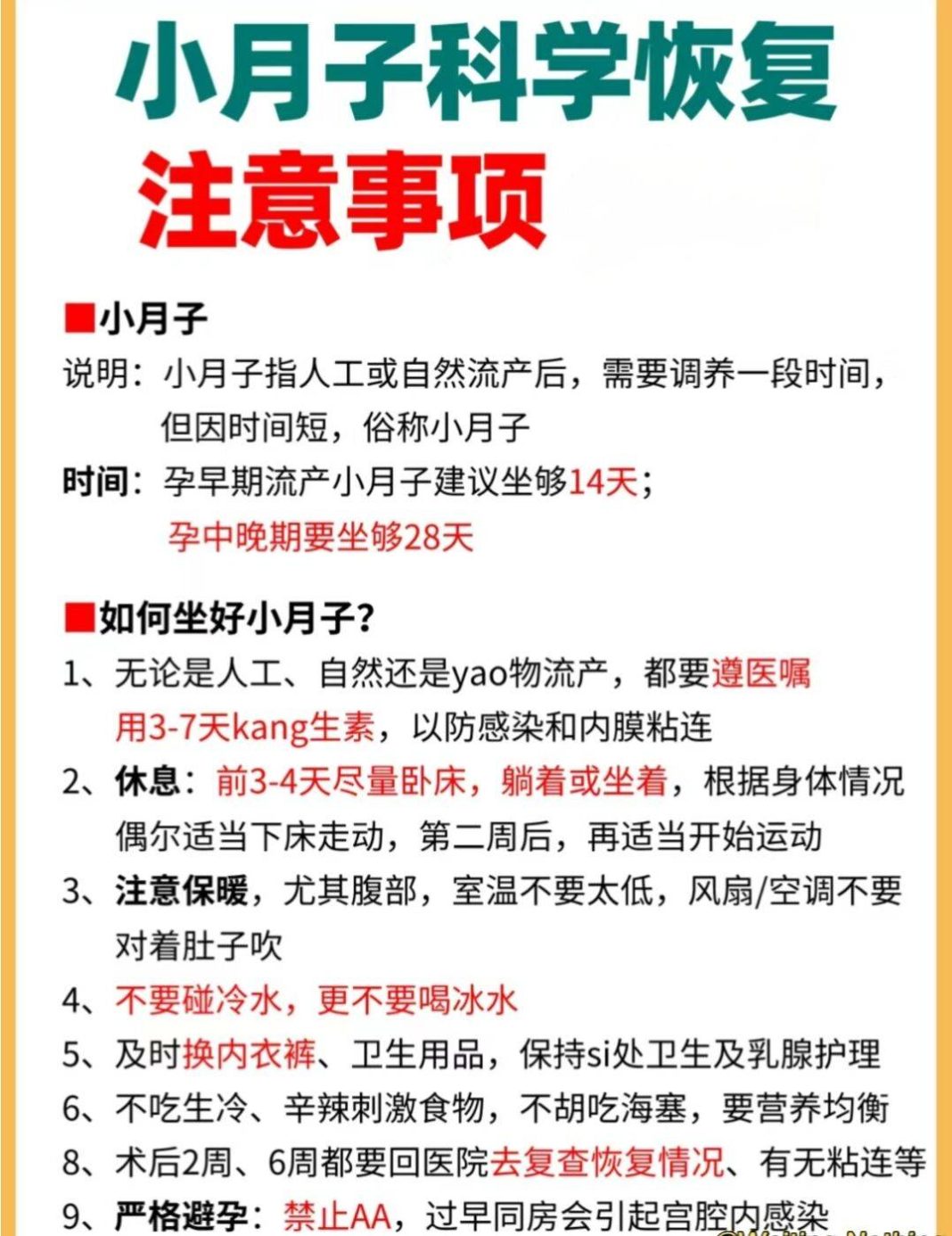
After abortion surgery, women should strictly follow medical advice for care and recovery. Maintain personal hygiene to prevent infections; ensure adequate rest and nutrition; undergo regular follow-up examinations to monitor body recovery.
3. Regular Check-ups
Regular gynecological examinations can help detect and treat potential reproductive system issues timely, preventing infertility. It is recommended that women undergo gynecological check-ups at least once a year.
4. Maintain a Positive Mindset
Maintaining a positive and optimistic mindset is crucial for increasing fertility. Women should learn to adjust their emotions and mindset, avoiding excessive anxiety and tension.
Difficulty in conceiving after a miscarriage is not an incurable condition. With scientific treatment and proper care, most women can fulfill their fertility desires. When facing this issue, women should remain calm and rational, seek medical help promptly, identify the cause, implement targeted treatment, improve lifestyle habits, maintain a positive mindset, and cherish their health to avoid the adverse effects of unnecessary abortion surgeries. (What should women do if they are unable to conceive after having one miscarriage?)