In recent years, antipsychotic drugs have played an important role in the treatment of bipolar disorders due to their clear efficacy and predictable safety. Currently, the combination of mood stabilizers and antipsychotic drugs has become the recommended first- and second-line treatment for bipolar disorders according to mainstream guidelines.
On the other hand, the phenomenon of using two antipsychotic drugs in combination to treat bipolar disorders is also common in clinical practice, sometimes even in the long term. This approach generally lacks sufficient evidence support, but objectively it can be beneficial for some patients.
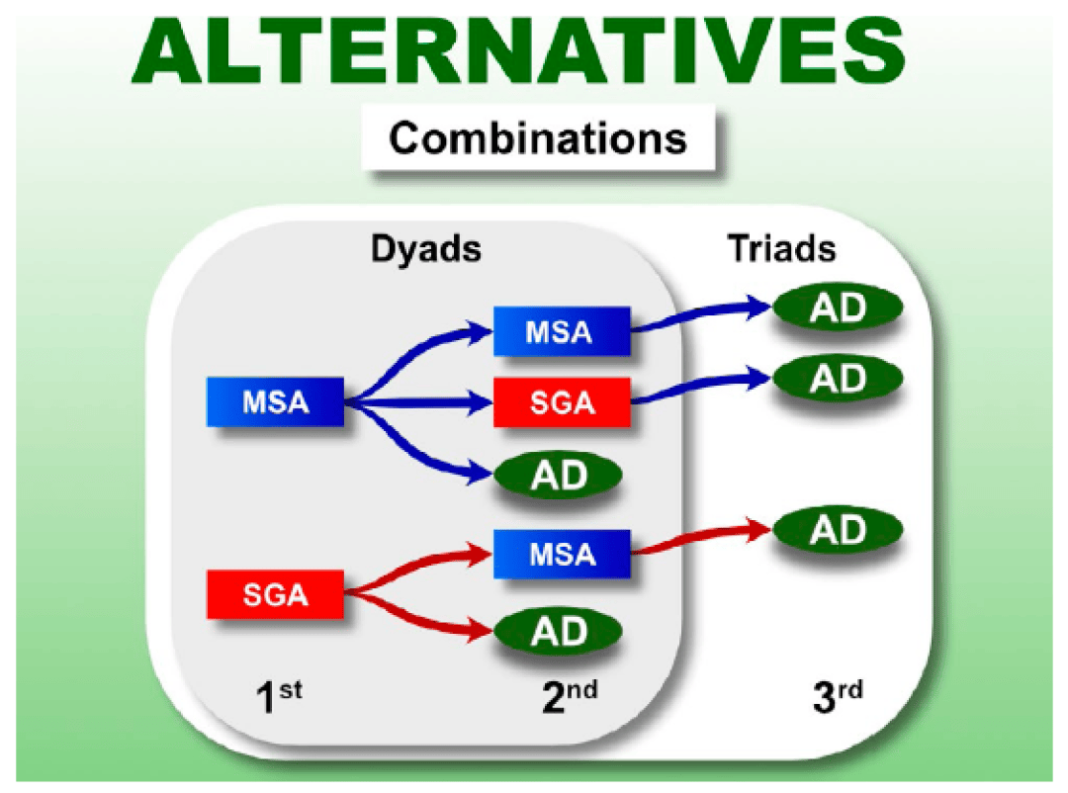
2020 RANZCP Mood Disorder Guidelines: It is not recommended to combine two second-generation antipsychotic drugs or two antidepressants for the treatment of bipolar depression; MSA, mood stabilizers; SGA, second-generation antipsychotic drugs; AD, antidepressants
In an article published online on July 29th in Bipolar Disord., a group of Brazilian researchers explored four relatively reasonable scenarios of using two antipsychotic drugs in combination to treat bipolar disorders:
Reasonable scenarios
1. Targeting different symptoms
A typical example is quetiapine. The pharmacological effects of this drug differ at different doses: low doses have a sedative effect, moderate doses treat mood episodes without psychotic symptoms, high doses act as antimanic and antipsychotic. Since quetiapine is a first-line treatment for manic and depressive episodes, if a patient has psychotic symptoms, it seems reasonable to use quetiapine to address mood issues on one hand and combine it with another antipsychotic drug to address psychotic symptoms on the other hand.
In addition, low-dose (e.g., 50mg/day) quetiapine can effectively improve sleep problems, including enhancing sleep quality and increasing total sleep time. Therefore, using low-dose quetiapine to improve sleep in patients with bipolar disorders is both common and reasonable, even if the patient is concurrently using another antipsychotic drug.
2. Treating refractory patients
In this case, combining a second antipsychotic drug may enhance efficacy and improve tolerability. A common situation is refractory mania, where clinicians may combine high-potency D2 receptor antagonists (e.g., haloperidol, fluphenazine) to control mania. However, this approach should not be routine, as evidence supporting this practice is limited and primarily derived from patients with schizophrenia rather than bipolar disorder.
3. Improving side effects
A typical example is combining aripiprazole to reduce prolactin levels. Research results show that compared to placebo, combining 5, 10, 20mg/day of aripiprazole can significantly improve risperidone-induced hyperprolactinemia.
When the pharmacokinetics of antipsychotic drugs differ, combining these drugs to achieve a diversified receptor action spectrum may benefit some patients. For example, combining aripiprazole with clozapine can improve negative symptoms and alleviate certain adverse effects, such as weight gain and elevated prolactin levels. Combining two D2 receptor antagonists may lead to increased prolactin levels, but the patient’s insomnia may be less severe.
4. Long-acting injectables in combination with oral medications
In some countries, long-acting injectable antipsychotic drugs are also approved for treating bipolar disorders. For patients who benefit from long-acting injectable treatments but have poor compliance, combining oral medications may be considered. In this case, long-acting injectables can serve as a safety net to prevent destabilization if the patient discontinues oral medications.
Recommendations
Although combining antipsychotic drugs poses safety risks, including an increased risk of long-term cardiovascular events, it is important to consider that these adverse outcomes may not necessarily be related to combination therapy itself but rather to the potentially high total drug dosage after combination.
Additionally, when combining antipsychotic drugs, it is crucial to evaluate the rationality of each drug in the regimen. Each drug used for bipolar disorder patients has its own level of evidence, including specific evidence for different clinical phases (mania vs. depression vs. mixed), phases (acute vs. maintenance), refractory cases (refractory vs. non-refractory), and comorbid symptoms (e.g., anxiety), and should be carefully assessed without hasty decisions.
Table 1 Reasonable combinations of antipsychotic drugs and the value of further research
Although there are many combinations of antipsychotic drugs, information on the overall efficacy or efficacy for specific symptom clusters, regarding the relative risk-benefit profiles of these combinations, remains limited. Therefore, it is necessary to restrict the use of combined antipsychotic drug therapy in patients with bipolar disorders, such as limiting it to a few scenarios mentioned above. Future studies should explore these combinations (Table 1) while taking into consideration the complexity of real-world patients.
References: Gnielka V, Roza TH, Passos IC. Should we combine antipsychotics in patients with bipolar disorder? Bipolar Disord. 2024 Jul 29. doi: 10.1111/bdi.13482. Epub ahead of print. PMID: 39075023.
Is it reasonable to use two different antipsychotic drugs to treat bipolar disorder?