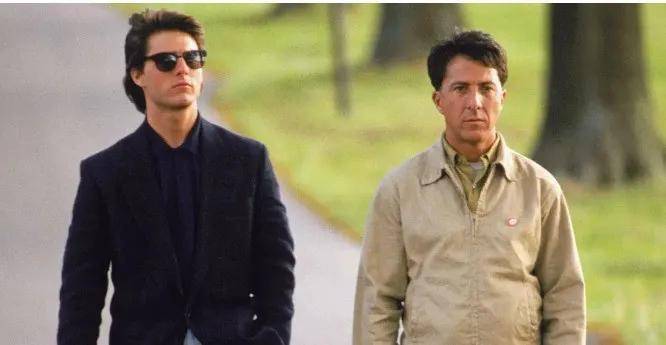
In the 1988 film “Rain Man,” Dustin Hoffman plays Raymond, an autistic patient with a tilted head and vacant gaze. At times, his eyes even fail to align, and he avoids eye contact when conversing, effectively portraying his inner emotional changes. This depiction captures the image of an “autistic” patient who is “half idiot, half genius” vividly, allowing people to understand that such individuals exist in society.
During the early stages of neural development, there is a close interaction between the nervous system and the immune system. Scientists speculate that neural inflammation, minor glial cell activation, and abnormal immune regulation may be key factors leading to autism in most patients.
Therefore, immune modulation therapy is currently being used in the treatment research of autism in children.
Mesenchymal stem cells (MSCs) are undifferentiated pluripotent stem cells proven to regulate neural inflammation, provide neural protection, and enhance synaptic function.
In preclinical in vitro models, MSCs can inhibit T-cell responses and reduce glial cell activation. Therefore, MSCs are promising candidate therapeutic agents in the treatment of neurological diseases.
This study recruited 12 autistic children aged 4-9, divided into 3 groups for dose escalation research. The children received 1-3 treatments each.
Assessments were conducted at 6 and 12 months post-treatment completion, using the VABS-3, PDDBI, and CGI-I scales, completed by patients’ families and clinical physicians.
The results showed that 50% of patients (6/12) showed improvement in at least 2 of the 3 assessments, while 33% (4/12) showed improvement in all 3 assessments.
Clinical Case Studies
According to a study published in the Journal of Translational Medicine in 2013, treatment of 15 autistic children with mononuclear cells combined with umbilical cord MSCs yielded outcomes significantly better than traditional rehabilitation training in the placebo control group. The authors of this study include Lyu Yongtao et al.
In a study published in Stem Cells Translational Medicine by Riordan et al. in 2019, results indicated improvement in assessment outcomes after treating 20 autistic children with umbilical tissue-derived MSCs.
On May 19, 2020, data from a study led by Joanne Kurtzberg et al. showed that after umbilical cord blood MSC treatment in 180 autistic children, the subgroup without intellectual disabilities exhibited improved language communication, increased focus, and enhanced brainwave activity.
Intellectual disabilities may affect disease prognosis, and similar phenomena have been observed in the treatment of other neurological conditions like cerebral palsy.
The Pediatrics Department of Wuhu City People’s Hospital collaborated with the Navy General Hospital Pediatrics Department to explore the safety and effectiveness of stem cell transplantation in treating autistic children. They administered human neural precursor cells and bone marrow-derived mesenchymal stem cells to 9 autistic children each.
After transplantation, 13 out of 18 children showed improvement in social skills, language abilities, and fine motor functions. Notably, none of the 18 children experienced severe adverse events, indicating that stem cells are effective and safe for low-functioning autism.
Summary: Recent studies have found that inflammatory immunity has an inhibitory effect on neurogenesis, especially in the hippocampus. Stem cells can regulate immunity and exert anti-inflammatory effects to counteract this inhibition.
Stem cell transplantation technology has shown promising therapeutic effects in various neurological disorders, suggesting that stem cell therapy for autism is advancing rapidly. It aims to provide a colorful world for more children and families, allowing individuals from afar to gradually feel the warmth and love of the Earth.