Being infected with bacterial vaginosis is essentially a reduction or disappearance of lactobacilli in the vagina, leading to a rise in vaginal pH, an imbalance in vaginal microflora, and excessive growth of other microorganisms, mainly anaerobes such as Gardnerella, Prevotella, Streptococcus, as well as Mycoplasma, resulting in bacterial vaginosis.
Statistics indicate that the infection rate of bacterial vaginosis falls between 15% to 50%; although the cure rate within one week is 80% to 90%, the recurrence rate within three months is 15% to 30%.
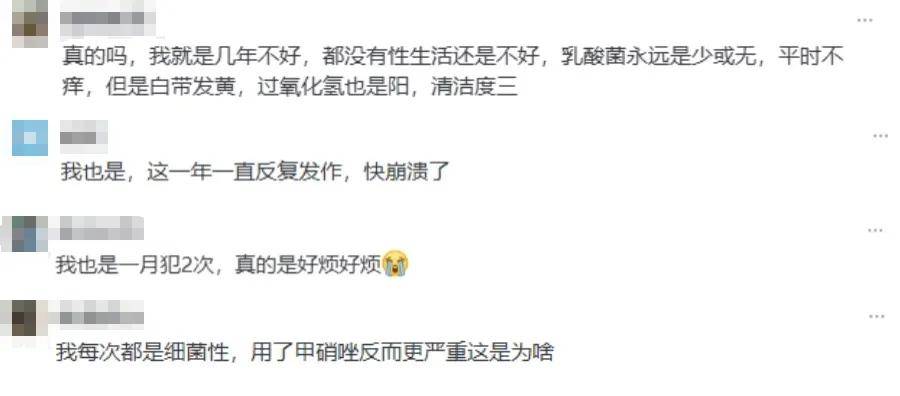
On social media, it is common to come across cases where despite multiple treatments, some individuals still struggle with recurrent infections!
If the pathogen is identified and treated correctly, this disease is not very difficult to combat. Common causes of recurrent infections include improper medication usage, incomplete treatment, failure to fully restore the balance of vaginal flora, and other detailed reasons as explained below.
Traditional bactericidal irrigation therapy involves the use of antibiotics, washes, etc.
The main characteristic of antibiotics and washes is their rapid killing of pathogenic bacteria, visibly alleviating symptoms. However, antibiotics not only eliminate pathogenic bacteria but can also affect beneficial lactobacilli in the vagina.
Overuse of drugs can disrupt the balance of vaginal flora, leading to vaginal dysbiosis and recurrent vaginitis. Prolonged and excessive use may result in drug resistance, making future treatment of vaginitis more challenging.
Many individuals, after using antibiotics or washes, experience a significant relief in symptoms and mistakenly believe they are cured, thus discontinuing the medication themselves. When the vaginal microenvironment has not yet fully recovered to its healthy state and lacks the protection of lactobacilli, pathogens can easily take advantage and cause recurrent vaginitis.
Therefore, after bactericidal treatment, it is essential to promptly replenish lactobacilli with vaginal probiotics. This process is akin to recruiting reinforcements immediately after eliminating disease-causing bacteria, establishing protective dominance of beneficial bacteria, ultimately restoring the balance of vaginal flora and reducing the recurrence of vaginal infections.
With the widespread adoption of vaginal microflora balancing therapy, many female friends have also come to understand the importance of replenishing lactobacilli to restore vaginal flora and prevent recurrent inflammation. However, the variety of lactobacilli is vast, with some being ineffective and potentially delaying the best treatment period, resulting in unnecessary expenses.
Oral probiotics
Oral probiotics for women are claimed to be specifically tailored for female health, improving gynecological inflammation and avoiding various vaginal infections. However, the primary target of oral probiotics is the intestines rather than the vagina, so their effectiveness in preventing vaginal infections is not significant.
Product with no formal approval or dietary supplements
Even though some female friends are aware that treating vaginitis requires the local supplementation of vaginal lactobacilli, not all realize the distinction between dietary supplements and medications. Choosing dietary supplements or unapproved products delays the optimal treatment period and exacerbates inflammation if not promptly addressed.
Therefore, for treating vaginitis with lactobacilli, it is advisable to select products with proper certification from national pharmaceutical authorities.
For bacterial vaginosis, in addition to conventional treatment, supplementing with vaginal probiotics to restore the lactobacilli-dominated weakly acidic environment is crucial in reducing recurrent vaginal infections. A novel microbiota therapy approach represented by lactobacilli, known as “bacteria against bacteria” and “bacteria-driven bacteria,” effectively adjusts the disrupted vaginal microflora environment, restores the weakly acidic environment of the vagina, and enhances local vaginal immunity.
Moreover, even if symptoms disappear during treatment, it is essential to follow medical advice, ensure timely, adequate, and proper medication.
[Reference]
[1] Fan Aiping. Clinical Diagnosis of Bacterial Vaginosis, Mixed Infection, and its Relationship with Mycoplasma. Diss. Tianjin Medical University.