It is unclear when exactly the prostate became a vital “gland” in men’s lives; it seems that if something goes wrong with it, men can no longer be “men”.
This can probably be attributed to the countless telephone poles, televisions, and mobile phones that indicate how important the prostate is, making you constantly aware of its health, and any discomfort triggers excessive anxiety.
But, do you truly understand the prostate? Let’s take a look at these 5 small questions about the prostate!
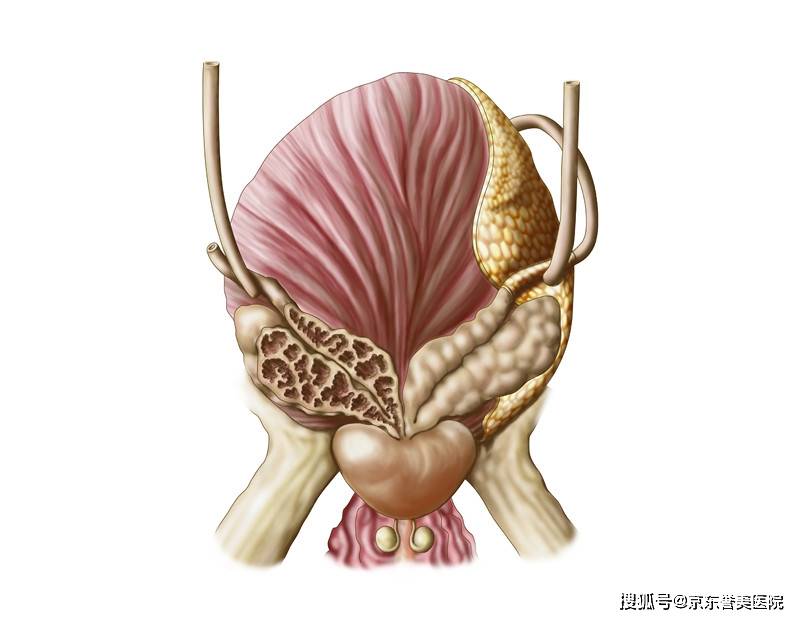
1. Where is the prostate?
A Near the anus (**)
B Near the testicles (testes)
C Near the banana (**)
Interpretation: A Near the anus (rectum)
The prostate is very close to our “anus”; it resembles a full, smooth chestnut and is hidden deep within the pelvic cavity, located beneath the bladder, connected to the bladder outlet (bladder neck), with the urethra passing through the middle; the left and right ejaculatory ducts also enter from above, creating two “T intersections”.
2. Does sitting for long periods affect prostate health?
A Yes
B No
Interpretation: A Yes
Prolonged sitting not only “compresses” the prostate but also slows down blood circulation, causing the prostate to be in a state of “congestion”.
If a sitting position is maintained for a long time, the secretion from the prostate can easily block the gland ducts, potentially triggering chronic prostatitis.
Therefore, taking timely breaks at work to “fish around,” grab a glass of water, or stretch a bit is highly beneficial for protecting our prostate~
3. Is frequent urination, urgency, incomplete urination, or split urine a sign of prostate problems?
A Yes
B No
C Not necessarily
Interpretation: C Not necessarily
Although frequent urination, urgency, incomplete urination, split urine, or difficulty urinating are indeed major symptoms of prostatitis and prostate enlargement.
Clinically, there are many causes for symptoms like urgency and frequency. Urologists need to inquire about medical history and conduct routine prostate fluid tests to reach a conclusion.
Prostatitis is fairly common and has variable symptoms, with unclear mechanisms of occurrence; it often lingers and recurs, and is not necessarily a separate disease but a group of syndromes, which is why it is often blamed.
4. Does chronic prostatitis affect sexual life?
A Yes
B No
C Not necessarily
Interpretation: C Not necessarily
From an anatomical and physiological perspective, the prostate is unrelated to functions like erection. There is no clear evidence that chronic prostatitis leads to erectile dysfunction.
Why do we often hear that “prostate inflammation impacts sexual function”?
This might be attributed to two reasons:
n Patients experience significant psychological stress, along with anxiety, depression, insomnia, and memory decline. They hear various “theories” and then self-doubt and self-suggest, leading to identifying with the negative aspects;
n Patients may encounter localized pain and urinary abnormalities, which can impact their sexual life.
If a man has “issues,” the prostate is not usually the main culprit.
5. Does prostatitis affect fertility?
A Yes
B No
C Not necessarily
Interpretation: C Not necessarily
The relationship between prostatitis and infertility is still undecided; clinically, most patients with prostatitis have normal fertility. The claim that “prostatitis causes infertility” is exaggerated in rumors.
Theoretically, prostate fluid is an important component of **, promoting ** liquefaction and enhancing sperm survival and transport. Therefore, if a patient suffers from prostatitis, the quality of ** may be affected, but it does not lead to infertility. Moreover, with proper treatment, most patients achieve good recovery outcomes.
Some say that prostatitis is like a “cold” of the prostate and not a major illness. While this is not entirely accurate, there’s no need to panic or feel anxious about the condition; timely and proper treatment should be sought, avoiding trust in misleading advertisements, and one should not feel ashamed or hesitant to seek medical attention.
Note: Any diagnostic or medicinal knowledge mentioned in this article is for reference only and should not be considered clinical diagnostic basis.