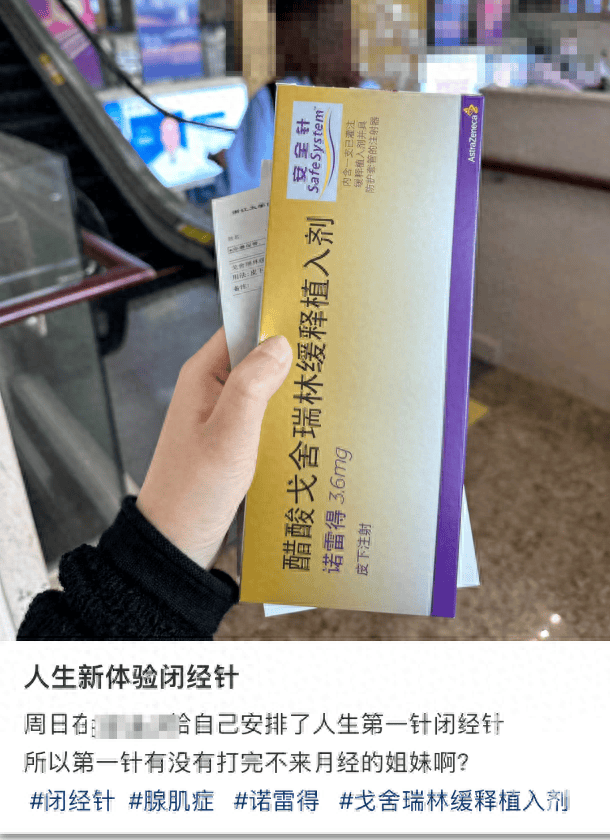
“Last Sunday, I arranged for myself the first injection of the menopause injection. Have any sisters not had their period after the first injection?” A netizen posted on Xiaohongshu.
This post sparked a lot of discussion among netizens, with many stating that they are also getting the injection. Some netizens expressed curiosity whether after receiving the “menopause injection,” they could indeed experience menopause and avoid some of the awkwardness that comes with menstruation.
Has been used clinically for over 20 years
Primarily used to treat
various gynecological diseases and precocious puberty in children
What is the “menopause injection”? Dr. Xu Ping, deputy chief physician of the Department of Gynecology at the Affiliated Hospital of the Medical College of Zhejiang University, explained that the “menopause injection” is a biodegradable polymeric controlled-release implant that gradually degrades in the body, releasing synthetic gonadotropin-releasing hormone (GnRHa). It has been used clinically for over 30 years to treat endometriosis, adenomyosis, breast cancer, abnormal uterine bleeding, and more.
Dr. Xu Ping mentioned that in addition to common gynecological diseases, GnRHa is also used in assisted reproduction and the treatment of precocious puberty. In children with precocious puberty, the use of GnRHa can suppress sexual development, reduce abnormally elevated hormones, and delay bone age maturation.
After the injection, it’s as if entering menopause early
Not recommended if no disease is present
“In the clinic, I have encountered some girls who consult about dealing with major exams or important events, asking if they can delay their periods. Many of them also mentioned the menopause injection,” Dr. Xu Ping said, noting that for such patients, the “menopause injection” is not recommended due to its significant side effects.
One netizen shared their experience of receiving the “menopause injection” to treat endometriosis. They said, “One injection every 28 days, each injection costing 1500 RMB. After the second injection, menstruation stopped and only resumed six months later. It was very uncomfortable during that period, experiencing night sweats, becoming easily angered. Finally, I understand the impact of hormones on women during menopause.”
Dr. Xu Ping introduced that GnRHa comes in agonist and antagonist forms. GnRHa agonists are injectable, typically administered every four weeks or every three months for the long-acting form. Usually, by the second injection, menstruation stops, leading to a state of “pseudo-menopause.” GnRHa antagonists can be taken orally and are already on the market abroad, undergoing clinical trials domestically and expected to be available soon.
Dr. Xu Ping mentioned that after receiving the “menopause injection,” it’s like simulating an early menopausal state. The inhibitory effect of GnRHa on the pituitary gland is very strong, leading to a significant decrease in estrogen levels in the body, causing symptoms like hot flashes, sweating, mood swings, vaginal dryness, and sleep disturbances resembling perimenopausal symptoms. Women lacking estrogen protection are at risk of bone loss, coronary heart disease, and increased risk of brain disorders.
When using GnRHa to treat conditions, calcium supplementation, minor estrogen supplementation, and other treatments are typically administered simultaneously. Prolonged use is not recommended, and treatment generally lasts less than six months.
Want to delay your period?
You can try oral contraceptives
If you only need to delay menstruation for special occasions, you don’t need such potent medications. Dr. Xu Ping suggests opting for progestins or oral contraceptives, which have relatively mild effects on hormones and fewer side effects. By continuously taking oral contraceptives until you want your period to start, stopping for 2-3 days will induce menstruation.
Regardless of the method used, it is important to note that without specific circumstances, do not easily alter your menstrual cycle. Furthermore, whether using oral contraceptives or progestins, there is a possibility of treatment failure; when externally supplemented progestins cannot fully counteract internal hormonal changes, menstruation will still occur normally.
Source: Chen Shi Interactive – Urban Express Journalist: Wu Shuang