In our daily lives, there are many topics that are considered taboo, often avoided in conversation. Among them, male sterilization is a particularly sensitive topic.
However, for the sake of scientific health, it is necessary to break this taboo and let everyone understand what happened to those men who did undergo sterilization. Has their quality of life changed? How is their physical health? Let’s discuss these questions together.
I. Basic knowledge of male sterilization
1. Definition of male sterilization
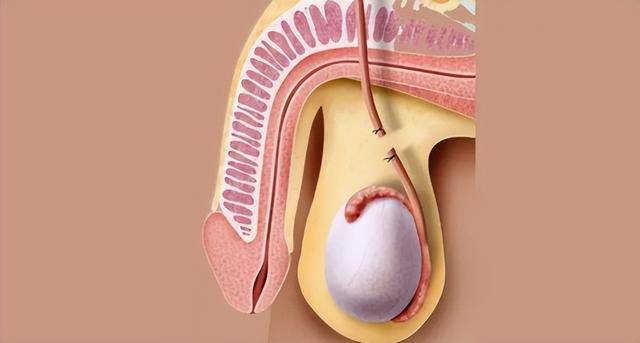
Male sterilization, also known as vasectomy or sterilization surgery, is a common long-term contraceptive method for men. It is a surgical procedure that involves cutting and sealing the vas deferens to prevent sperm from the testes from reaching the urethra, thus achieving contraception. This procedure is usually reversible, but not all cases can be successfully reversed.
2. Process of sterilization surgery
Male sterilization surgery is typically performed in a doctor’s office or operating room under local anesthesia. During the surgery, the doctor makes a small incision in the scrotum, locates the vas deferens, and cuts it.
The cut ends of the vas deferens are sealed, possibly through methods like cauterization, clamps, sutures, or using special connectors. The surgery usually takes 20 to 30 minutes. There may be mild discomfort post-operation, but most men can resume normal activities within a few days after surgery.
3. Purpose and effects of sterilization
The main purpose of male sterilization is as a long-term or permanent contraceptive method. For men who do not intend or no longer wish to have children, sterilization is an effective choice.
The success rate of sterilization surgery is very high, with a very low likelihood of failure. However, it should be noted that sterilization does not take effect immediately because there may still be sperm in the semen post-surgery. Multiple semen analyses are usually needed in the months following surgery to ensure the absence of sperm in the semen.
Furthermore, sterilization does not prevent sexually transmitted diseases, so protective measures are still necessary in risky sexual activities.
II. Physiological effects of male sterilization
(I) Impact on fertility
1. Infertility after sterilization: Male sterilization is a common contraceptive surgery that prevents sperm from entering the ejaculate by cutting or blocking the vas deferens, thus rendering men infertile.
2. Reversibility of sterilization and vasectomy reversal surgery: Although theoretically male sterilization can be reversed through vasectomy reversal surgery, the actual success rate is not very high. The success rate of reversal surgery depends on factors such as the duration since sterilization, surgical techniques, the age of the male, etc.
(II) Impact on sexual function
1. Effects of sterilization on libido and sexual performance: Male sterilization does not affect libido and sexual performance. The surgery simply cuts or blocks the vas deferens without affecting male hormone secretion, thus it does not affect libido and sexual performance.
2. Impact of sterilization on sexual life: Men after sterilization can have normal sexual intercourse and do not have to worry about accidental pregnancies, which may make their sexual life freer and worry-free for couples who do not intend to have more children.
(III) Impact on health
1. Possible complications post-sterilization: Sterilization surgery is a minor operation with low surgical risks. However, like any surgery, there is a possibility of complications such as infection, bleeding, pain, etc. In addition, some men may experience psychological discomfort post-sterilization, such as anxiety, depression, etc.
2. Relationship between sterilization and prostate cancer, cardiovascular diseases, etc.: Current scientific research has not confirmed a direct relationship between male sterilization and prostate cancer, cardiovascular diseases, among others.
Sterilization surgery does not affect male hormone secretion, so theoretically it does not increase the risk of these diseases. But if men lead unhealthy lifestyles post-sterilization, such as unbalanced diet, lack of exercise, they may still increase the risk of developing these diseases.
III. Psychological effects of male sterilization
1. Impact on self-identity: Men may experience an impact on their male identity post-sterilization. In many cultures, fertility is seen as an important part of male power and identity. Therefore, losing fertility may make some men feel diminished self-worth and may even trigger a crisis in self-identity.
2. Impact on sexual life satisfaction: Male sterilization does not affect their sexual function or libido. However, if they misunderstand the surgery or feel anxious about losing their fertility, it may affect their satisfaction with their sexual life. On the other hand, not having to worry about accidental pregnancies post-sterilization may increase their sexual life satisfaction.
3. Impact on partner relationships: Male sterilization may affect their relationships with their partners. If partners have different views on the surgery, it may lead to conflicts. On the other hand, if the partner supports this decision, it may strengthen their relationship as it shows the male taking responsibility to prevent unplanned pregnancies.
4. Impact on future fertility plans: Male sterilization is a permanent contraceptive method, so for men who are certain they do not want children, it is an effective choice. However, if they change their minds post-surgery and want to reproduce again, they may feel regret and disappointment.
Although it is possible to reverse sterilization through surgery, the success rate is not very high and the cost is expensive. Therefore, men need to carefully consider their future reproductive plans before deciding on sterilization.
IV. Conclusion
Overall, male sterilization surgery is an effective, safe contraceptive method. The surgery does not impact male libido, sexual performance, or significantly affect the quality of life.
However, men should fully understand the risks and potential psychological impacts of the surgery before deciding to undergo sterilization surgery to make the most suitable decision for themselves.