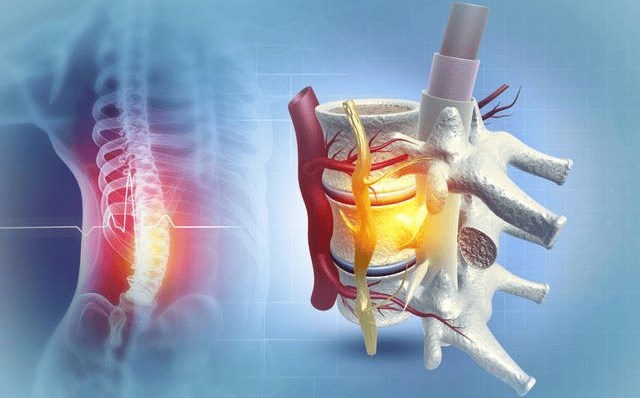
Spinal Cord Injury
☛ The incidence varies in different countries
☛ 12-50 cases per 1,000,000 in Europe and America, 39.4 cases per 1,000,000 in Japan, 68 cases per 1,000,000 in China
☛ Most common in young adults, male-to-female ratio is about 3.5:1
☛ Main causes include falls from heights, traffic accidents, crushing by heavy objects, violence-induced injuries, etc.
☛ Falls are the primary cause of injuries in people aged 60 and above
Etiology
☛ Traumatic: major causes include car accidents, falls, violence, sports accidents, acrobatic accidents, industrial accidents, natural disasters, whip-induced injuries, etc.
☛ Non-traumatic: inflammation, vascular, degenerative changes, developmental abnormalities, tumors, etc.
Mechanism
☛ Closed injuries: trauma causing excessive extension/flexion or torsion of the spine
☛ Open injuries: caused by burst injuries, firearm injuries, fractures piercing the spinal cord, etc.
☛ Whiplash injuries: a specific type of neck spinal cord injury
☛ Non-traumatic: compression, infection, ischemia, immune-related, etc.
Clinical Presentation
Rehabilitation Treatment
Traditional Rehabilitation Goals
Level of Injury
Ability to Perform Activities
Ability to Perform Daily Life Activities
C1-C3
Dependent on the diaphragm for breathing,
Able to control certain activities by voice
Entirely dependent
C4
Use of electric high-back wheelchairs, controlled by mouth or jaw,
Sometimes requires assistance with breathing
Mostly dependent
C5
Able to manually move a high-back wheelchair on flat surfaces,
Requires upper limb assistive devices and specially modified wheelchairs
Moderately dependent
C6
Able to manually operate a wheelchair, independently dress,
get in and out of bed, and enter/exit vehicles,
Capable of driving specially modified vehicles
Partial dependency
C7
Wheelchair use, able to independently transfer to bed/chair/
toilet/bathroom
Mainly self-reliant
C8-T4
Able to manually operate a wheelchair,
use pelvic braces to stand,
Basic self-reliance
I
Motor Function Rehabilitation
☛ Residual bodily function training
☛ Use of assistive devices to improve motor skills
☛ Prevention of secondary complications
II
Respiratory Function Rehabilitation
☛ Standing training
☛ Respiratory muscle strength training
☛ Assisted coughing, cough training
☛ Postural drainage, mechanical vibration, percussion, mechanical cough assistance
☛ Cardiovascular management
III
Neurogenic Bladder Rehabilitation
☛ Standing
☛ Intermittent catheterization with a reasonable drinking plan
☛ Prevention of urinary tract infections: asymptomatic bacteriuria does not require treatment
☛ Acidic urine can inhibit microbial growth
☛ Flushing with ample urine inhibits microbial attachment
☛ Coordinate with medication to achieve the “balanced bladder” goal
☛ Prevention of urolithiasis
☛ Functional training for small bladders
IV
Pressure Ulcer Management
☛ Identify the cause of the injury, eliminate or reduce risk factors
☛ Regularly reposition, thoroughly cleanse wounds, change dressings
☛ Improve nutrition, enhance overall health
☛ Maintain skin cleanliness, dryness, use flat bedsheets
☛ Avoid dragging, pulling, pushing, and similar movements
☛ Local use of pressure patches or transparent patches
☛ Vacuum sealing drainage treatment for wound closure (VSD)
☛ Intelligent pressure relief mattresses, cushions
☛ Management of pressure injuries related to medical equipment (oxygen tube, tracheostomy tube, urinary catheter, nasogastric tube, respiratory mask)
V
Occupational Rehabilitation
Injury
Level
Training Goals
Training Plans
Injury at C5
Using aids for eating;
Using voice-controlled electric wheelchairs;
Assisted bed-to-chair transfers
Strength training, self-feeding aids
Use, long sitting, balance, range of motion
Injury at C6
Manual turning, sitting up;
Dressing in simple clothing by oneself;
Using a tripod or crossbar for transfers;
Using gripping aids to pick up objects
Manual turning, sitting up training,
Strength training, wheelchair driving training,
Transfer training
Injury at C7
Basic self-care;
Independently performing pressure relief while sitting;
Various transfer actions with a slider
Movement training,
Various transfer training,
Strength training
Injury at C8-T1
Independent bed activities;
Independent wheelchair activities;
Independence in toileting;
Independently dressing, writing, using communication tools
Upper limb strength and endurance training,
Sitting pressure relief training,
Wheelchair rear-wheel balance and
Street crossing skills using a wheelchair
Operational technique training
VI
Other Functional Rehabilitation
☛ Orthostatic hypotension: application of abdominal belts, elastic stockings, SGB, pressor agents, high-salt diet, orthostatic bed training
Autonomic reflex abnormality: removal of harmful stimuli, nifedipine tablets, nitroglycerin ointment, etc.
☛ Pain: 60%-70% of SCIs have neuropathic pain, treatment with physical factors, SGB, medication, psychotherapy
☛ Deep vein thrombosis: rehabilitation thinking between rest and activity; prevention as the main approach; elevation, anticoagulation, thrombolysis, passive exercise, avoidance of intravenous fluid infusion in lower limbs; interventional therapy
☛ Heterotopic ossification: standardize rehabilitation behavior; once detected, stop movement at ossification sites, physical factors (cold therapy, heat therapy), bisphosphonates application, surgical treatment
VII
Rehabilitation of Activities of Daily Living
☛ Basic ADLs include: various movements (turning, sitting up, transferring), eating, dressing, grooming, bathing, toileting, etc.
☛ Instrumental ADLs include: housework, transportation use, shopping, wheelchair or walking aid maintenance, reading, etc.
☛ Combined with hand function
☛ Partially compensate for function using self-help tools and hand supports
☛ Assistance from environmental control systems and nursing robots
Neurorehabilitation Department
Our neurorehabilitation department primarily utilizes physical therapy, exercise therapy, occupational therapy, speech therapy, rehabilitation engineering, etc. The department combines advanced rehabilitation concepts and technologies from Europe and America with traditional Chinese medicine acupuncture and massage, providing comprehensive rehabilitation treatment for musculoskeletal injuries, central and peripheral nerve lesions, chronic pain, etc.
The department focuses on muscle strength training, endurance training, joint function training, joint loosening procedures, nerve stimulation procedures, balance function training, hand function assessment and training, activities of daily living assessment and training for neurological system lesions (spinal cord injury, cerebrovascular disease, traumatic brain injury, cerebral palsy, peripheral nerve injury).
Department Features
Cerebral Palsy in Children
Stroke Rehabilitation
Musculoskeletal Disease Rehabilitation
Neurological Disease Rehabilitation
Comprehensive Rehabilitation of Post-Traumatic Brain Injury Syndrome
Arousal Therapy for Comatose Patients
Respiratory and Rehabilitation Training for High-Level Spinal Cord Injuries
Swallowing Dysfunction Training, Cognitive Dysfunction Training
Rehabilitation of Paralysis and Urinary Dysfunction Caused by Trauma or Spinal Cord Lesions
Rehabilitation of Geriatric Diseases such as Dementia, Parkinson’s Disease, and Cerebellar Atrophy
Expert Introduction
Zhou Zhiqiang
Director of Neurorehabilitation Department
Chief Physician
Former Chief Physician of Neurology Department, Chongqing People’s Hospital
Former Deputy Director of the Stroke-Induced Depression and Mental Disorders Sub-Committee of the Chongqing Stroke Association
Member of the Psychosomatic and Behavioral Disorders Sub-Committee of Chongqing Medical Association
Member of the Sleep Disorders Study Group of the Neurology Sub-Committee of Chongqing Medical Association
Member of the Neurological and Mental Disorders Study Group of the Psychiatric Medicine Sub-Committee of Chongqing Medical Association
City-level Review Expert for Speech Disabilities
Review Expert for “Laboratory Medicine and Clinical Practice” Journal
Published over 10 medical papers
Contributor to the book “Geriatric Dementia”
Specialties: Proficient in degenerative diseases such as stroke, hemiplegia, paralysis, Parkinson’s disease, and senile dementia; intracranial infectious diseases, multiple sclerosis; peripheral nerve diseases (diabetic peripheral neuropathy, alcoholic peripheral neuropathy, Guillain-Barre syndrome); diagnoses and treatments for various headaches, insomnia, anxiety, depression, and psychosomatic disorders; epilepsy and muscle diseases.