The six hormonal tests include: Estradiol (E2), Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH), Progesterone (P), Testosterone (T), and Prolactin (PRL).
Estradiol (E2):
Estrogen is one of the main hormones produced by the ovaries, playing a crucial role in maintaining female reproductive function and secondary sexual characteristics. The estrogen tested in the six hormonal tests mainly refers to Estradiol (E2). Normal E2 levels are considered in cases of uterine amenorrhea, while lower results may suggest primary or secondary ovarian insufficiency or anovulatory cycles. Non-cyclical E2 levels are commonly seen in anovulatory functional uterine bleeding, polycystic ovary syndrome, or certain postmenopausal uterine bleeding. Measuring E2 while administering medication for ovulation can monitor follicle development, maturation, and ovulation status.
Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH):
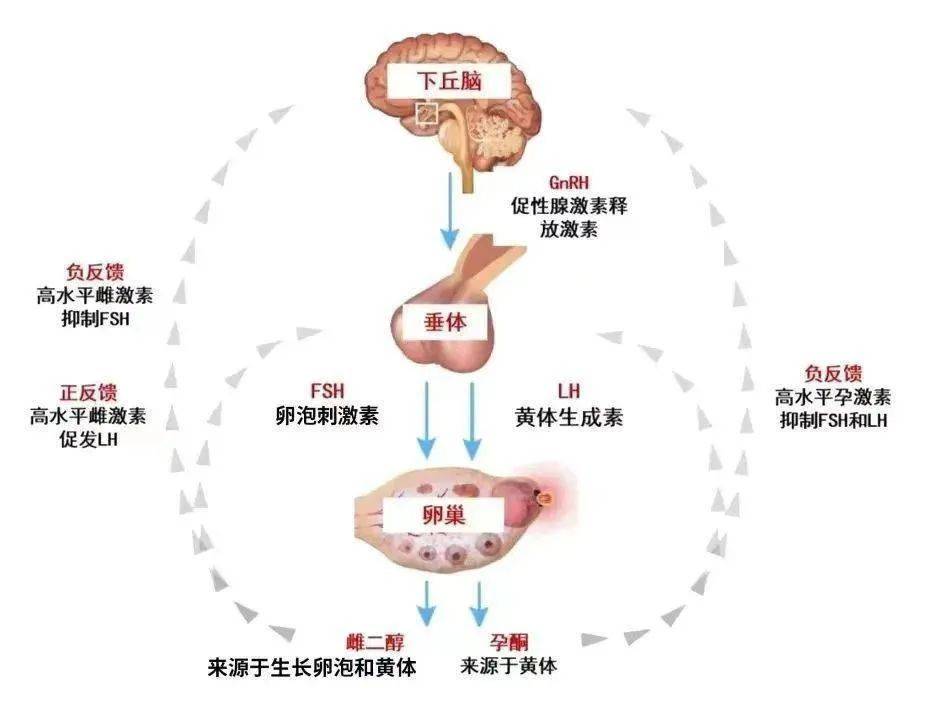
The physiological function of LH primarily promotes ovulation and luteal formation, stimulating the secretion of progesterone and estrogen. FSH’s physiological function promotes follicular maturation and estrogen secretion. Levels of LH and FSH can help determine the cause of amenorrhea: low levels suggest possible hypothalamic or pituitary issues; high levels indicate potential ovarian pathology. Measuring LH peak can estimate ovulation status, aiding in the treatment of infertility.
Progesterone (P):
When LH surge occurs, the ovaries begin to secrete progesterone, and serum progesterone levels increase steadily during pregnancy. Progesterone can be used to monitor ovulation; if progesterone reaches ovulation levels and there are no other causes for infertility, ultrasound monitoring of follicle development and ovulation should be conducted to rule out luteinized unruptured follicles. In cases of anovulatory menstruation, anovulatory dysfunctional uterine bleeding, primary or secondary amenorrhea, and polycystic ovary syndrome, progesterone levels may decline. During the luteal phase, reduced progesterone levels indicate luteal insufficiency, and high progesterone levels on days 4-5 of menstruation suggest incomplete luteal regression. In ectopic pregnancies, progesterone levels are relatively low; declining progesterone levels during pregnancy suggest placental insufficiency; decreasing levels during threatened miscarriage indicate a possibility of miscarriage.
Testosterone (T):
In women, T primarily derives from the conversion of dehydroepiandrosterone secreted by the ovaries and adrenal glands. Elevated T levels can lead to masculinization and hirsutism, although normal T levels may indicate sensitivity of hair follicles to androgens. Abnormal increases in T can occur in conditions such as adrenal cortical hyperplasia or tumors and poorly differentiated endometrial cancer.
Prolactin (PRL):
PRL is a peptide hormone secreted by the lactotrophic cells of the pituitary gland, acting on breast cells to promote the growth and differentiation of glandular tissue. PRL should be tested in cases of amenorrhea, infertility, and menstrual irregularities to exclude hyperprolactinemia. Pituitary tumors accompanied by elevated PRL suggest the possibility of prolactinoma.