One, About Breast MRI
As a malignant tumor with a high incidence rate among women globally, breast cancer poses a significant threat to women’s health. Epidemiological studies have shown that the incidence of breast cancer is showing a trend towards younger age groups related to economic development levels and educational levels. Statistical data shows that in populations of women with high living standards and higher educational levels, there is a significant increase in the incidence of breast cancer, making breast cancer screening an important topic in the public health field.
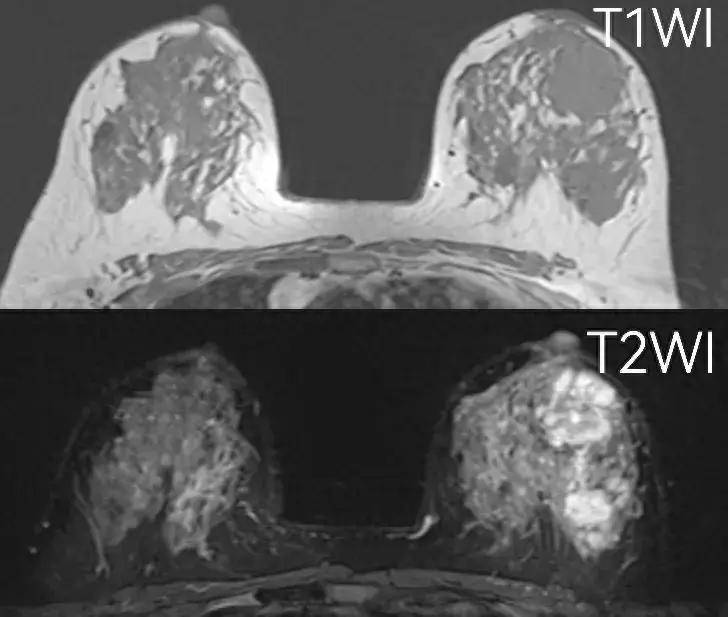
With the advancement of breast cancer detection technology, although traditional X-ray imaging and ultrasound examinations are widely used clinically, they still have their limitations. Especially in the detection of early breast cancer and identification of small lesions, these methods may not fully meet clinical needs. Therefore, breast magnetic resonance imaging (MRI) technology is increasingly being adopted in more clinical research and practices due to its superior soft tissue contrast resolution and high sensitivity.
Breast MRI examination uses a powerful magnetic field and radio wave signals to provide detailed images of breast tissue without using radiation. The significant advantage of this technology is its ability to finely characterize the internal structure of the breast, especially for women with dense breast tissue, MRI can effectively differentiate breast tissue from potential lesions. In addition, MRI shows high accuracy in evaluating the tumor size, morphology, and its impact on surrounding tissues in known breast cancer patients, which is of great value in guiding surgical strategies and treatment plan development.
At the molecular level, breast MRI can also provide the tumor’s hemodynamic characteristics and microenvironment features through functional imaging techniques such as diffusion-weighted imaging (DWI) and dynamic contrast-enhanced imaging (DCE-MRI), further revealing the tumor’s biological behavior. This information is crucial for assessing the invasiveness of the tumor, prognosis, and treatment response.
Two, Who Should Have a Breast MRI Examination?
1. Breast cancer diagnosis
When breast X-ray imaging or ultrasound examination is unable to determine the nature of the lesion clearly, MRI examination can provide higher resolution images to assist doctors in further diagnostic analysis.
2. Breast cancer staging
MRI shows high sensitivity in assessing the spread of breast cancer. It can effectively identify multicentric or multicenter lesions that are difficult to detect by other means and can detail whether cancer has invaded surrounding structures like the breast fascia or pectoralis major muscle. This function is crucial in formulating surgical plans, especially in breast-conserving surgery.
3. Evaluation of neoadjuvant chemotherapy efficacy
For breast cancer patients receiving neoadjuvant chemotherapy, conducting MRI examinations before, during, and after chemotherapy can effectively evaluate the patient’s response to chemotherapy and the status of residual lesions after chemotherapy.
4. Lymph node metastasis in the axilla without known primary lesion
In cases where axillary lymph nodes show metastasis without finding the primary lesion, MRI can help explore the primary cancer lesion hidden in the breast, providing a basis for further treatment decisions. Additionally, negative MRI results can rule out the possibility of a primary breast lesion, avoiding unnecessary treatment interventions such as total mastectomy.
5. Monitoring recurrence after breast-conserving surgery
For breast cancer patients who have undergone breast-conserving surgery, routine clinical and imaging examinations may not accurately determine whether the condition has recurred. MRI can effectively differentiate recurrent tumors from scars formed after surgery in this respect.
6. Post-breast reconstruction follow-up
For patients who have undergone breast implantation, traditional X-ray imaging may not provide sufficient diagnostic information. MRI can evaluate the status of implanted prostheses and assist in diagnosing breast cancer.
7. Screening high-risk individuals
For high-risk groups, individuals with a family history of breast cancer, MRI can detect breast cancer that may be missed by other examinations, especially when clinical and ultrasound examinations fail to show any abnormalities.
8. MRI-guided biopsy
When traditional imaging techniques cannot clearly locate the lesion, performing a biopsy guided by MRI can improve the accuracy and safety of the biopsy.
Three, Who are the High-Risk Groups for Breast Cancer?
The American Cancer Society (ACS) defines the high-risk group for breast cancer to include the following:
1. Carriers of BRCA gene mutations, where the risk of developing breast cancer can reach 60% to 80%, and the risk of ovarian cancer is 40%. The high-risk age group for this population is 40 years old, and regular screenings are recommended starting from the age of 30. Additionally, individuals carrying BRCA1 gene mutations are more sensitive to radiation.
2. According to the ACS guidelines, individuals with a lifetime risk of breast cancer of 20% to 25% or higher are recommended for breast cancer MRI screening, including those who have undergone chest radiation therapy, such as Hodgkin’s disease patients.
Four, What are the Disadvantages of Breast MRI Examination?
1. Patients with metallic implants in their bodies cannot undergo MRI imaging.
2. Patients allergic to contrast agents used in MRI should not undergo such examinations.
3. Patients with claustrophobia, due to the confined space during MRI scanning, may feel uncomfortable and are not recommended for this examination.
4. Patients who cannot lie prone are not suitable for magnetic resonance imaging.
5. Compared to other breast examinations, the cost of magnetic resonance imaging is usually higher.
Five, When is Breast MRI Examination Generally Conducted?
1. 7-14 days after the end of menstruation (to avoid physiological enhancement);
2. 6 months after surgery;
3. 12 months after radiotherapy;
4. 4-6 weeks after stopping hormone replacement therapy.
Six, What Precautions Should be Taken During Breast MRI Examination?
Experts from Hunan Provincial Hospital of Traditional Chinese Medicine remind patients that during this examination, patients need to assume a prone position, the entire process lasts about 15 to 20 minutes, and fasting is required for two hours before the examination. After the examination, it is recommended to increase water intake, as about 90% of the contrast agent will be excreted unchanged in the urine within 24 hours. Additionally, to reduce the impact of hormonal levels during the menstrual cycle on detecting breast lesions falsely, it is recommended to undergo the examination in the 2nd to 3rd week after the end of the menstrual period, with the 2nd week being the optimal time.
In conclusion, breast magnetic resonance imaging (MRI) is a very useful diagnostic tool, especially suitable for breast diseases that are difficult to diagnose through conventional imaging techniques. It plays an important role in diagnosing, staging breast cancer, assessing treatment effectiveness, and cancer screening in high-risk populations.
However, it should be noted that breast MRI is not suitable for everyone, especially for patients with metallic implants, allergies to contrast agents, or claustrophobia. Moreover, the cost of MRI is higher compared to other breast examination methods. Therefore, before choosing to undergo a breast MRI examination, patients should thoroughly understand their health conditions, the indications for MRI, the optimal timing for the examination, and relevant precautions to make the most appropriate medical decisions.
Article by Hunan Provincial Hospital of Traditional Chinese Medicine, Department of Medical Imaging, Gan Qixin
Follow @Hunan Medical Chat for more health information!