Uterine cavity adhesion occurs when the basal layer of the endometrium is damaged due to factors such as injury or infection, preventing the endometrium from repairing itself, leading to hyperplasia of fibrous connective tissue, causing the walls of the uterine cavity to adhere to each other, narrowing or even blocking the cavity.
The primary cause of uterine cavity adhesion is procedures performed within the cavity, particularly in the case of abortions or dilation and curettage surgeries. In recent years, with the popularity of painless abortions, the incidence of uterine cavity adhesions has also been increasing, mainly because under anesthesia, the uterine muscles relax, the uterus softens, and the tactile feedback for the operating physician diminishes. Additionally, patients under anesthesia are unable to provide feedback to allow doctors to adjust the pressure applied during the procedure, increasing the likelihood of endometrial injury. Furthermore, conditions such as infections and tuberculosis can also lead to uterine cavity adhesions.
If the following situations occur, vigilance is needed for early diagnosis and treatment, as more favorable outcomes can still be achieved.
1. For those with a history of regular menstrual cycles, if menstruation does not resume 40 days after an abortion or postpartum weaning, they should promptly seek medical attention to rule out the possibility of uterine cavity adhesion.
2. Reduced menstrual flow after an abortion or medical abortion curettage.
3. A history of intrauterine surgeries with accompanying infertility or recurrent miscarriages.
4. A past history of endometritis or pelvic tuberculosis with decreased menstrual flow.
5. Multiple ultrasound examinations indicate a thin endometrium.
What are the dangers of uterine cavity adhesion? The primary concern is infertility.
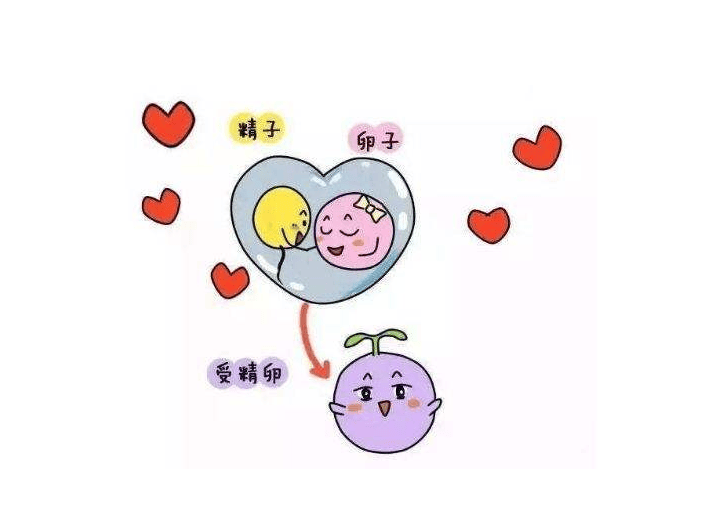
In reproductive medicine, there is a metaphor of “seed” and “soil,” where the “seed” refers to the fertilized egg and “soil” refers to the endometrium. When there is uterine cavity adhesion, the endometrium becomes thin, and some areas may lack any endometrial tissue, making the “soil” impoverished, and it is very difficult for the unfortunate fertilized egg to find a suitable place to implant.
Severe uterine cavity adhesions can lead to occlusion of the uterine corners or cervix and blocking of the fallopian tubes, preventing sperm from combining with the egg. Additionally, uterine cavity adhesions may cause irregular uterine contractions, potentially leading to a miscarriage.
Can in vitro fertilization (IVF) be performed with uterine cavity adhesions?
If the adhesions are mild, treatment may not be necessary, and IVF can proceed directly, as the impact is not particularly significant. If a hysteroscopy is needed, it is advisable to begin the IVF process first, meaning to stimulate the ovaries for egg retrieval and obtain sperm from the male partner, then cultivate the embryos but not implant them initially. After properly resting and optimizing health, perform the hysteroscopy, and conduct the embryo transfer when recovery is satisfactory and there is no cycle of recurrence of adhesions. This can enhance the embryo implantation rate. Therefore, patients must cooperate promptly with medical treatment to strive for an early recovery.