A couple of days ago, a reader asked about what vaginal spasm is all about.
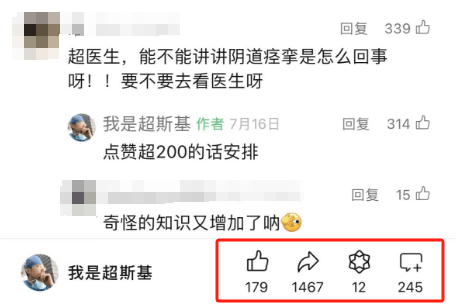
srds, what I said was that an article with over 200 likes will be scheduled for posting. As a result, everyone started praising in the comments section, and everyone enthusiastically liked and shared to repost, which fueled my writing spirit~ This time, it was my fault for not making it clear, so I had to write it even with tears, 55555.
What is “vaginal spasm”?
We often hear about male sexual dysfunctions, but female sexual dysfunctions also exist. Yes, “vaginal spasm” is a relatively rare type of “female sexual dysfunction” (FSD). Research reports a clinical incidence rate of about 5% – 7% for “vaginal spasm,” but due to the nature of this condition, the actual incidence rate may be higher.
The term “vaginal spasm” was coined by James Marion Sims in 1862. According to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) issued by the American Psychiatric Association in 2000, “vaginal spasm” is defined as “repeated or sustained involuntary spasms of the outer 1/3 of the vaginal muscle tissue, interfering with sexual intercourse and causing pain and difficulties in interpersonal relationships.” The characteristics of dyspareunia include genital and/or pelvic pain.
Due to the difficulty in distinguishing between these two conditions, they were merged into “Genitopelvic Pain/Penetration Disorder” in the DSM-5.
PS: I’m thoughtful, providing the English translation for everyone to learn.
What are the symptoms of “vaginal spasm”?
The most common clinical manifestation of vaginal spasm is difficulty in vaginal penetration, often associated with fear or emotional distress. Since excessive fear of sexual pain is a common symptom in patients, vaginal spasm is also known as “banana phobia syndrome.”
Some women experience severe tension, anxiety, fear, pain, and discomfort when attempting vaginal penetration with a penis or similar object. In addition to involuntary spasms of the outer 1/3 of the vagina, which closes the vaginal opening, some individuals may even tightly close their legs to protect the perineal region.
Essentially, during attempts at intercourse, some women find it difficult to spread their thighs apart, and even if they do, due to the contraction of vaginal muscles, they feel like they are “hitting a wall” and cannot penetrate anything inside.
If a woman exhibits at least one of the following symptoms, “Genitopelvic Pain/Penetration Disorder” should be considered:
– Significant, persistent, or repeatedly occurring sexual penetration difficulties, including involuntary tightening or spasm of the pelvic floor muscles during attempts at penetration;
– Obvious, persistent, or repeatedly occurring external genital or pelvic pain or discomfort before, during, or after penetration;
– Significant, persistent, or repeatedly occurring fear or anxiety of external genital, vaginal, or pelvic pain before, during, or after penetration.
Despite having sufficient sexual desire and stimulation, these symptoms repeatedly occur during sexual interactions involving or possibly involving penetration.
What are the different types of “vaginal spasm”?
“Vaginal spasm” can be classified as primary and secondary, complete and situational.
Primary vaginal spasm is more common, occurring from the initiation of sexual relationships, with these individuals rejecting any form of vaginal penetration. In contrast, secondary vaginal spasm refers to cases where individuals had a normal sexual history but later developed vaginal spasm due to various factors.
Complete vaginal spasm refers to the inability to complete penetration of a penis or similar object on any occasion, while situational vaginal spasm indicates tolerance for certain types of penetration, such as tampons or speculums, only becoming tense during penis penetration. It can also refer to tolerance in some scenarios or with certain partners but an inability to tolerate penetration in other scenarios or with other partners, resulting in different manifestations according to different situations.
What causes “vaginal spasm”?
Currently, there is no clear cause for vaginal spasm. Most researchers and clinicians believe that vaginal spasm is a psychophysiological issue involving cognitive, behavioral, and physiological factors.
On one hand, psychological factors play a role, such as inadequate sexual education from a young age, consciously or unconsciously associating sexual activities with shame, embarrassment, anxiety, fear, and guilt; some individuals may have heard from friends that intercourse causes pain or even heavy bleeding, or may have a history of painful experiences during intercourse leading to a fear-related memory, all contributing to the development of vaginal spasm. Additionally, some individuals may develop a fear of intercourse due to rough behavior by male partners causing intense pain and trauma.
The Fear-Avoidance Model of Pain is often used to explain the occurrence of vaginal spasm, describing how negative experiences with penetration behavior lead to negative sexual experiences and the subsequent development of a fear of penetration.
Furthermore, gynecological conditions that can cause sexual pain may also trigger vaginal spasm, such as thickening and toughening of the hymen (vaginal valve), scarring and narrowing of the vagina, vulvar inflammation combined with ulcers in the vulvar or vestibular region, endometriosis, and senile atrophic vaginitis.
What impact does “vaginal spasm” have on sexual life?
Due to the tight closure of the vaginal opening during intercourse, the male partner is completely unable to enter. In the continuous attempts, the male partner may become flaccid, potentially leading to a misdiagnosis of “erectile dysfunction.”
I have encountered some cases in my clinical practice where some individuals had been diagnosed with “erectile dysfunction” when they actually had partners with vaginal spasm.
When male partners seek treatment, they may say, “I have trouble with erections, I can’t penetrate the vagina during intercourse, and I often go soft when trying to enter the vagina.” “This is my wife’s first time, I don’t have much experience either. After trying several times without success, I got nervous, the more nervous I got, the less erect I became, and eventually, I couldn’t get hard anymore.”
I asked the male partners, “Have you tried using your hand to assist your partner, can your finger enter?”
“Not really, as soon as we prepare to enter, she tenses up all over. Initially, I thought she might be nervous and scared because it’s her first time, so her lower body is also tight. Later, I found out that even my fingers cannot get in, and using lubricant doesn’t help either.”
After relevant examinations and interviews, it was determined that the male partners had no major erectile issues; the problem mainly lay on the female side.
I advised the female partners to seek gynecological care. They later informed me that when the gynecologist attempted to perform a pelvic exam, there was noticeable tension in the thighs and vaginal area.
In another case, a male partner was also distressed by “erectile dysfunction,” attempting numerous times to penetrate the vagina without success, leading to the penis becoming flaccid due to repeated failed efforts. After consulting various urologists and being advised to take medications like “Viagra,” as well as undergoing treatments, he still couldn’t engage in intercourse. Seeking a male specialist, he was even recommended to undergo a “penile prosthesis” surgery, but the high cost of the procedure ultimately deterred him. After consulting with me and understanding the situation, I asked about the female partner’s condition, discovering that she exhibited symptoms of “vaginal spasm” every time they attempted intercourse, leading to continuous failure. After the female partner sought gynecological treatment, the situation improved, and eventually, they were able to engage in intercourse.
Since this condition is not very common, and female partners may feel reluctant to seek medical attention, timely diagnosis may not be obtained when symptoms occur, potentially leading to difficulties in engaging in sexual activities and affecting fertility.
Therefore, if women experience any of the aforementioned clinical manifestations, they should remember to visit a public hospital gynecologist for assessment to avoid worsening the condition.
Now, many readers are probably wondering how to treat or improve vaginal spasm. If the article receives over 200 likes, we will discuss this next time!
References
[1]Spector IP, Carey MP. Incidence and prevalence of the sexual dysfunctions: a critical review of the empirical literature.Arch Sex Behav. 1990;19(4):389-408.
[2]Raveendran AV, Rajini P. Vaginismus: Diagnostic Challenges and Proposed Diagnostic Criteria.Balkan Med J. 2024;41(1):80-82.
[3]Chinese Association of Plastic and Aesthetic Medicine Technology Innovation and Organ Restoration Branch. Chinese Expert Consensus on the Diagnosis and Treatment of Female Sexual Dysfunction (2023 version).Chin J Obstet Gynecol. 2023;58(9):641-649
Disclaimer: Some images are from the internet. Please contact for removal if any infringement occurs.