When it comes to statins, they should be very familiar to most cardiovascular patients. Numerous clinical studies have shown that statins play a very significant role in lowering cholesterol, regulating blood lipids, and stabilizing the risk of cardiovascular diseases.
However, many people have always had the concept of “medicine has three points of poison,” feeling that although statins are good, they are afraid of causing hidden dangers to health by taking them every day. Therefore, they are curious about how long they need to take this medication to complete a course of treatment and whether they can stop taking the medication after lowering their blood lipids.
01
Is it necessary to take statins if you have high blood lipids?
Whether a patient with high blood lipids needs to take statins depends on the specific condition of the patient. If it is only high blood lipids without other complications, medication may not be necessary.
By controlling diet, such as a low-salt, low-fat, low-cholesterol diet, eating more vegetables and fruits, avoiding overwork, late nights, smoking, alcohol, controlling weight, and exercising properly, blood lipids can generally be controlled.
If a condition of high blood lipids is accompanied by coronary heart disease, hypertension, diabetes, cerebral infarction, cerebral hemorrhage, or other related vascular diseases, medication is needed, and statins are one of the choices.
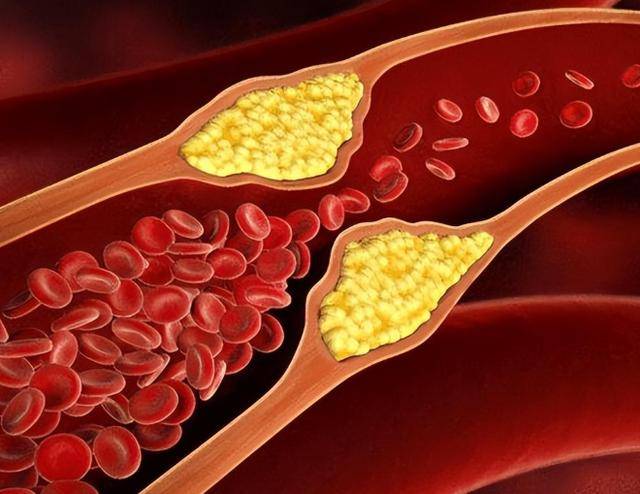
Because high blood lipids can cause blood viscosity, leading to thrombosis, arterial hardening, narrowing of blood vessels, and complications, a combination of lifestyle changes, diet adjustments, and medication may be needed to normalize blood lipids, possibly requiring long-term medication.
For patients with elevated cholesterol levels who do not have apparent atherosclerotic diseases, they may need to take statins, regularly monitor cholesterol levels, and consider discontinuing medication once the data stabilizes.
However, for patients with atherosclerotic diseases, regardless of elevated cholesterol levels, taking statins is generally recommended to stabilize plaque in blood vessels and prevent the progression of atherosclerotic diseases.
02
Taking atorvastatin to reduce blood lipids, how long does a course of treatment last? Can you stop taking the medication? The doctor analyzes the truth for you.
For many patients taking atorvastatin, a common concern is: how long should an atorvastatin treatment last? Can you stop taking the medication once your blood lipids return to normal?
After all, medications are a double-edged sword, and people always hope to avoid long-term medication dependency. However, there is no definitive “course of treatment” for atorvastatin.
Statins, such as atorvastatin, mainly work by inhibiting cholesterol synthesis in the liver to lower lipid levels. However, it is worth noting that this does not fundamentally solve lipid metabolism issues.
To maintain stable blood lipids, patients often need to take medication for an extended period. If medication is stopped without medical advice, the inhibitory effect on cholesterol synthesis in the liver may disappear, and lipid levels may rapidly rise again.
Although there is no fixed treatment duration, in certain special circumstances, stopping atorvastatin may be considered. When the following four indicators show abnormalities, patients should consult a doctor immediately:
First, if the serum creatine kinase level exceeds four times the normal value, caution is advised even if there are no discomforts; second, if muscle pain, weakness, or other symptoms occur, it could signal muscle damage;
Third, if the transaminase level is three times higher than the normal value, it is often a warning sign of liver damage; fourth, if the total bilirubin level is double the normal value, it could also indicate liver damage.
03
What are the long-term side effects of taking statins?
Gastrointestinal reactions: Statins may cause abdominal pain, diarrhea, nausea, vomiting, constipation, and other gastrointestinal discomfort.
Liver function abnormalities: Statins have hepatotoxicity and may damage liver cells, leading to elevated transaminases and liver function abnormalities. During the initial period of medication use, transaminase levels should be regularly monitored. If any functional abnormalities are detected, dosage reduction or discontinuation of medication is necessary.
Rhabdomyolysis: After long-term use of statins, patients may experience muscle pain. In such cases, creatine kinase levels should be examined. If levels are ten times higher than normal, the medication must be discontinued immediately to prevent rhabdomyolysis and potential kidney damage.
Glucose abnormalities: Mainly manifested as increased fasting glucose and glycosylated hemoglobin, diabetic patients may experience poor blood sugar control or worsening glucose levels.
Other systemic symptoms: Statins may also cause insomnia and rare allergic reactions, such as rashes, erythema, and so on.
Keep in mind that while statins may have side effects, they play a crucial role in regulating blood lipids, lowering the risk of cardiovascular diseases, and more.
Therefore, strict adherence to the doctor’s guidance, regular monitoring, and evaluation are necessary while taking statins to promptly adjust the treatment plan, ensuring the safety and efficacy of the medication.
04
Precautions for using statins
Diet adjustments: During medication, adhere to a low-fat diet, reducing intake of high-fat, high-cholesterol foods such as pork, lamb, butter, etc. Avoid oily, fried, spicy foods as they may affect the medication’s effectiveness.
Drug interactions: Statins have risks of interacting with other drugs. Inform the doctor about any other drugs used during statin therapy to prevent adverse reactions. For example, statins should not be used with cyclosporine soft capsules, itraconazole dispersible tablets, ketoconazole tablets, fenofibrate capsules, etc.
Observing side effects: Statins may cause muscle pain, liver function abnormalities, and other side effects. Therefore, regular liver function and muscle enzyme level checks are necessary during treatment. If any discomfort occurs, inform the doctor promptly to prevent deterioration of the condition.
Drug dosage: Patients should strictly follow the prescribed dosage, as both overdose and underdose can have adverse effects on health.
Considering that different types of statins and the same statin from different manufacturers may have variations in specifications and typical oral doses, be cautious about the specifications and dosages when switching medications.
Special populations: Pregnant and lactating women, patients with compromised liver function, muscle diseases, elderly individuals, etc., need special care when taking statins, and medical guidance is essential.
Clear indications for use: Statins are primarily used to treat high cholesterol levels, high lipoproteinemia, and can also be used for secondary prevention of coronary heart disease, ischemic stroke, etc. Before using statins, consult a relevant physician to confirm eligibility for treatment and avoid self-medication.